Drugs that block structural changes to collagen could prevent lung fibrosis
Scientists at the University of Southampton have found that it is the structure of collagen, rather than the amount, that drives progression of the devastating condition of lung fibrosis.
The study, published in the journal eLife, provides the first evidence in humans that altered collagen structure rather than collagen amount affects tissue stiffness during progression of lung fibrosis and identifies a potential new target for drugs to prevent the condition.
It is widely thought that fibrosis occurs when components that hold together a tissue’s architecture (called the extracellular matrix (ECM)) build up in the tissue and lead to tissue stiffness. But recently evidence has suggested that this increased stiffness causes the build-up of yet more ECM components, resulting in a cycle that causes more scar tissue.
In collaboration with Synairgen, a University of Southampton spinout company, and Pharmaxis, the Southampton team have used the results to develop a new compound to treat the structure of collagen, which is progressing to a Phase 1 clinical trial.
The interdisciplinary study involved researchers from Medicine, Engineering and the Institute of Life Sciences at the University of Southampton and was funded by the Wellcome Trust.
“We knew that stiffness is an important factor in the build-up of scar tissue in the lung,” explains lead author Mark Jones, NIHR Clinical Lecturer in Respiratory Medicine at the NIHR Southampton Biomedical Research Centre and University of Southampton.
“But we didn’t understand what specifically causes increased stiffness in diseased human tissue. Given that excessive build-up of collagen is considered a hallmark of fibrosis, we wanted to see whether this molecule has a role in tissue stiffness.”
They started by looking at the biological and mechanical features of lung tissue from people with lung fibrosis and compared this to healthy lung tissue. They found that the lung fibrosis samples were much stiffer than those from healthy people but, surprisingly, at time of diagnosis they had similar levels of collagen.
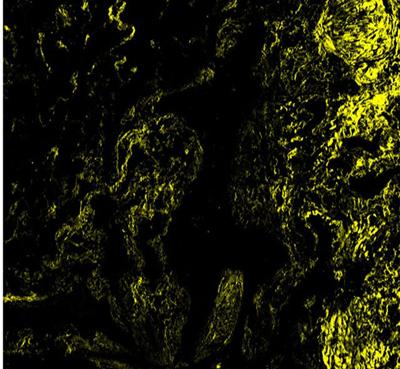
However, when they looked at enzymes that give collagen its unique ‘cross-linked’ structure within the ECM, they found that a family of these enzymes (the LOXL family) was more abundant in the fibrosis samples. This led them to further investigate the types of collagen structures found in the fibrosis samples – which are broadly grouped into immature and mature collagen cross-links. They found that increased lung tissue stiffness only occurred where there were higher amounts of the mature cross-linked collagen and that, in these samples, the structure of each collagen building block – or fibril – was altered. This suggested that it is collagen structure, controlled by the LOXL family, that determines tissue stiffness.
Having made this discovery, the team tested whether they could alter the structure of collagen by blocking the LOXL enzymes, with a view to preventing lung fibrosis. They tested a compound called PXS-S2A that blocks LOXL-2 and LOXL-3 in lung tissue cells isolated from people with fibrosis. They found that the number of cross-linked collagen molecules declined with an increasing dose of PXS-S2A.The compound also reduced tissue stiffness, even at low concentrations, suggesting that blocking LOXL-2/LOXL-3 could be an effective way to reduce tissue stiffness.
Finally, they tested the LOXL-2/3 inhibitor in rats with lung fibrosis and found that although there was no effect on total collagen content in the lungs, the treated rats had reduced fibrosis and improved lung function, with no adverse effects.
“Together, our results identify that treatment approaches which maintain normal collagen architecture may prevent tissue stiffening and limit the mechanisms that drive progressive fibrosis,” says Donna Davies, Professor of Respiratory Cell and Molecular Biology at the University of Southampton. “Our findings suggest the need to conduct studies in patients with lung fibrosis to see whether these approaches would be of benefit."