Targeting use of antibiotics in primary care through use of technology and better diagnostic assessment
Researchers in the Primary Care Research Centre (PCRC) at the University of Southampton have been addressing some of these challenges by conducting studies to develop and evaluate new diagnostic tests, and by developing and evaluating clinical prediction rules.
There are many reasons why antibiotics continue to be over-used in primary care. There continue to be strong societal beliefs about the role of antibiotics and lack of awareness about the risks of overuse. However, one of the key challenges has been inadequate diagnostic tools leading to diagnostic uncertainty. Diagnostic tests available to clinicians working in secondary care settings have generally not been available in a timely fashion in primary care. Primary care clinicians rely primarily on clinical skills, but evidence on the value of different clinical findings and how to combine them to improve diagnostic and prognostic accuracy, was lacking in the primary care setting.
The PCRC researchers sought to improve care by undertaking studies to develop and evaluate new diagnostic tests, and by developing and evaluating clinical prediction rules.
The NIHR HTA funded PACE research is just such a study on diagnostic testing. This study aimed to test whether a point of care C-reactive protein (CRP) fingerprick test could be used to safely reduce antibiotic use for patients presenting with an acute exacerbation of COPD [1].
Exacerbations of COPD can result in significant morbidity and mortality and are a common reason for hospital admission, so primary care prescribers have understandably taken a fairly liberal approach to the use of antibiotics in these patients. CRP is a marker of inflammation that tends to increase more in bacterial than viral infections. In the PACE study we were able to demonstrate that use of this test resulted in about a 70% reduction in antibiotics, with no evidence of prolonged illness or patient harm.
The research team in PCRC are now evaluating a point of care test (FebriDx) that combines CRP with a marker that is specific for viral infections in adults and children with respiratory tract infections in primary care [2]. PCRC researchers are also identifying new markers that could be developed into tests to improve the use of antibiotics in primary care. The NIHR School of Primary Care Research (SPCR) 4S study demonstrated that it was possible to measure markers of inflammation from throat swab samples in people with sore throats [3], and the NIHR SPCR DISCO-UTI study is evaluating new urinary biomarkers which may help identify urinary tract infection in care home residents [4].
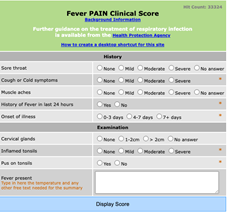
New diagnostic technologies show great promise, but ultimately clinicians need to bring together several pieces of diagnostic information to decide whether antibiotics are likely to be indicated or not. Clinical prediction rules (CPR) use scientific data to help clinicians make these decisions and researchers at PCRC have conducted research to develop CPR and demonstrate the value of these tools in primary care. A good example of this is the FeverPAIN score, developed by researchers at PCRC, which has now become the gold-standard tool for assessing the risk of Group A Strep (GAS) in people with throat infections [5]. This tool has been widely used around the world and has been particularly useful during the current wave of anxiety associated with an increase in invasive GAS in the U.K. Clinical prediction rules are useful in general practices but may also be useful in other primary care settings. The PCRC team are currently developing a digital tool with suite of CPRs for use by community pharmacists [6]. There is a strong push for community pharmacies to manage more acute infections, but it is essential that this does not lead to an increase in unnecessary use of antibiotics. This research aims to test whether pharmacy use of this digital suite of CPRs, combined with targeted diagnostic testing, leads to safe reductions in antibiotic use in the pharmacy setting.
For more information about research on use of antibiotics in primary care that is being led by the Primary Care Research Centre visit https://www.southampton.ac.uk/primarycare/research/index.page or contact
Professor Nick Francis nick.francis@soton.ac.uk
References
- Butler CC, Gillespie D, White P, Bates J, Lowe R, Thomas-Jones E, Wootton M, Hood K, Phillips R, Melbye H, Llor C, Cals JWL, Naik G, Kirby N, Gal M, Riga E, Francis NA. C-Reactive Protein Testing to Guide Antibiotic Prescribing for COPD Exacerbations. N Engl J Med. 2019 Jul 11;381(2):111–20.
- The PREFIX study — NIHR School for Primary Care Research [Internet]. [cited 2022 Dec 22]. Available from: https://www.spcr.nihr.ac.uk/research/projects/the-prefix-study
- Lown M, Miles EA, Fisk HL, Smith KA, Muller I, Maund E, Rogers K, Becque T, Hayward G, Moore M, Little P, Glogowska M, Hay AD, Stuart B, Mantzourani E, Butler C, Bostock J, Davies F, Dickerson I, Thompson N, Francis N. Self-sampling to identify pathogens and inflammatory markers in patients with acute sore throat: Feasibility study. Front Immunol [Internet]. 2022 [cited 2022 Dec 22];13. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2022.1016181
- DISCO UTI — NIHR School for Primary Care Research [Internet]. [cited 2022 Dec 22]. Available from: https://www.spcr.nihr.ac.uk/research/projects/disco-uti
- Little P, Moore M, Hobbs FDR, Mant D, McNulty C, Williamson I, Cheng E, Stuart B, Kelly J, Barnett J, Mullee M, Investigators on behalf of the P. PRImary care Streptococcal Management (PRISM) study: identifying clinical variables associated with Lancefield group A β-haemolytic streptococci and Lancefield non-Group A streptococcal throat infections from two cohorts of patients presenting with an acute sore throat. BMJ Open [Internet]. 2013 Oct 1 [cited 2020 Jan 8];3(10). Available from: https://bmjopen.bmj.com/content/3/10/e003943.
- STOP AMR — NIHR School for Primary Care Research [Internet]. [cited 2022 Dec 22]. Available from: https://www.spcr.nihr.ac.uk/research/projects/stop-amr