Localised use of antibiotics to improve infection management
Annually, an ever increasing number of people are having to undergo surgeries to remodel or replace joints such as knees, hips and shoulder due, largely, to an ageing global population. Known as total joint arthoplasties (TJAs), approximately 1-4 % of all of these surgeries result in infection, a serious complication with a devastating impact on patient health, high death rates and a large financial burden on the health service.
To prevent and treat infection, patients are given antibiotics which spread through the body in an attempt to kill the causative bacteria. However, in TJAs, there is a lack of blood supply to the surrounding area and the artificial joint, which often makes treatment ineffective as the antibiotics can not successfully reach the surgical site. This allows the infiltrating bacteria to grow and establish biofilms, large clusters of bacteria which are extremely difficult to treat with normal antibiotic intervention strategies. Moreover, poor treatment and an inability to completely eradicate an infection may also permit the remaining bacteria to develop antimicrobial resistance (AMR), further reducing the chances of successfully clearing the infection.
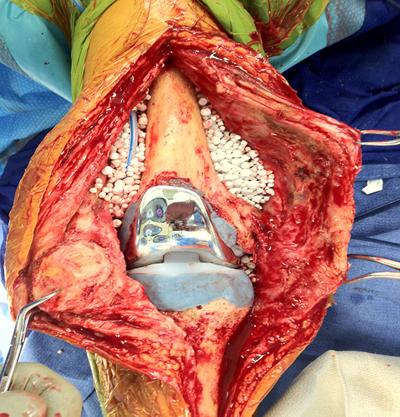
Image 1 shows joint replacement surgery with dissolvable antibiotic loaded beads to combat infection

This project is investigating the therapeutic benefit of delivering antibiotics directly to the surgical site using specialised carrier materials which, after releasing their antibiotics, completely dissolve in the patient. This ability to release high doses of antibiotics exactly where they are required to prevent an infection taking hold may improve treatment and prevent the risk of AMR developing.In our work, we perform studies into the ability of the materials to release various antibiotics, therefore allowing us to treat a variety of infections, and their effect on the bacterial and biofilms themselves and the mechanisms behind their response.
Image 2 shows an xray of a joint post surgery with antibiotic beads in place (reproduced with permission from Biocomposites Ltd)
NAMRIP team
This project is led by Dr Rob Howlin (Senior Research Fellow and NAMRIP steering committee member affiliated with the Southampton NIHR Biomedical Research Unit) and Prof. Paul Stoodley (National Centre for Advanced Tribology, University of Southampton and Departments of Microbial Infection and Immunity and Orthopedics, The Ohio State University) in collaboration with the Centre for Biological Sciences (Prof. Jeremy Webb) and is funded by Biocomposites Ltd.
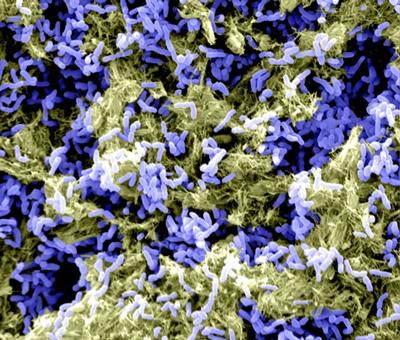
Image 3 is a scanning electron microscope image (false coloured where blue is the bacteria and yellow is the bacterial matrix) showing a biofilm of Propionibacterium acnes on orthopaedic implant material. Size of the rods is approx. 2 microns in length