Now that you have been on a few placements you may have been faced with a few more challenging aspects. We asked our students to share some of their experiences, and offer useful suggestions.
Amy
...in my first placement, if there was an audiologist that had been doing it for, you know, 30 years, they wouldn't really be told any differently, you couldn't really question them too much... Sometimes you have to say, "I'm really sorry, could you just explain this? Why are you doing that? What's this?" And sometimes if they can't answer you, I guess obviously they feel that they should be able to answer, and that's a little bit awkward if they can't.
Suggestions
- Amy should respect that they are a professional and should be careful not question them in front of a patient.
- Amy should ask them why they are doing it in that way and engage in a discussion of what they do and why they do it. They might have a good reason for choosing that particular approach!
- Amy should be open-minded and aware that they are a variety of approaches and methods. Everyone thinks differently. She should also remember of the protocols required for her exams.
- When this occurs it can be a little embarrassing for both parties too. Amy could offer to research an issue and report back. She needs to be diplomatic.
Rakesh
I'm also, more than anything, finding out that we get to see the emotional impact on a patient when you find out, oh dear, this patient doesn't actually want hearing aids, what do you do next? We're not taught that in a wet lab session of course, you know, you've just got a dummy in front of you and you talk to it.
Suggestions
- You will have patients that will break down and start crying. And at that point you might feel you are out of depth and that you need to go and find someone who can deal with this. Therefore, it will be good to observe how other professionals manage in such situations. If you see it happening while you are still observing, then write down how they managed it, reflect on it, and think about how you would have reacted so that you will be better prepared to deal with something similar in the future.
- Rakesh needs to make a judgement of the patient and the situation as every situation is different. For example, you can have patients who refuse or don't want to wear a hearing aid or they might feel obliged to wear it but really would not get on with it. He needs to talk to the patient and find out why they don't want a hearing aid.
- If this has just happened in an appointment, and you don't know what to do, then you have to hand it over. You can talk to a professional afterwards and discuss / reflect on the process.
Jennifer
I think actually when you get to a department and you don't know anybody and you've just about figured out where the toilets are and where the tea is, and then you sit there thinking, "What should I be doing?" and they'd go and look at me and think I'm not doing anything. I think that's quite tough. And yet what can you do? You don't know where anything is, you've got no experience. You don't want to suddenly volunteer to take on something and then them say, "You shouldn't have been doing that." So actually I think, to settle in, to be given something to do straight away is quite good.
Suggestions
- Once you have had a meeting with your supervisor and they've set out what they expect from you, anything that you do in addition to that should be something that you can handle and is manageable. If they give you something and you are unsure then ask for more instructions.
- If you find yourself on your first day with not very much to do, then go to your supervisor and ask them if there is anything else that you can do. But go to people with whom you have worked before and know your level and skills rather than someone you don't know.
- Jennifer should be proactive. If the supervisor is not around, she should go and find a senior person and ask for their induction plan / activities for the initial couple of days.
Erin
...people didn't necessarily like having a student with them, because it was inevitable that you were going to overrun. Because when you get more competent at things then you start to cut corners, so all the fully trained audiologists, they know how to do things, without compromising patient care, but they can do things a lot quicker. Whereas I'm sat there doing a hearing test exactly how I have to, because otherwise if you don't then they're like, "Oh you didn't do this properly," and, "Well I know, but look what time it is." So that got quite stressful sometimes.
Suggestions
- Remember you are there to learn and no one expects you to do it right especially when you are being watched. It is difficult though when you have a long list and you are trying to do everything according to the time boundaries. A way of managing it, it's perhaps to set yourself a small target for that appointment. In the next appointment you can try and fit in an additional goal. In that way you have got smaller goals to meet rather than the huge goal of doing the whole appointment in an hour.
- Erin needs to be careful about potentially picking up bad (and potentially unsafe) habits unawares. It is vital to learn how to undertake a procedure properly first.
- If you are having difficulty in one area, such as time management, talk to your supervisor and try and work out a way around that to help facilitate the difficulties you are having.
Jennifer
...there are some audiologists that you're with...they think the right way is the way they do it...So you kind of have to have a little bit of a memory that, you know, "I'm with this person, they like to do it like this."...I've said...I do it the way my supervisor has taught me because at the end of the day I'm going to have an assessment, and my supervisor is going to be in my assessment, and if I don't do it the way my assessor wants, my assessor will still pass me provided my supervisor sits there and says, "Well that's the way we've shown her, that's the correct way of doing it."...Basically I'm doing it the supervisor's way. But I've got a whole load of mental notes that when I'm qualified, and when I'm on my own, I kind of pick up a little bit from what they do and a little bit from this.
Suggestions
- This is so true and does happen! Jennifer has to find a style of working she feels comfortable with but it comes with time and experience.
- Jennifer should make a note of how they do it, ask them the reasoning behind it and use it as a prompt as she can never remember everything she learns on placement! She should also remember the protocols for her exams and do it correctly in her exams.
- Encountering lots of different practices means that students are likely to pick up tips and tricks of the trade, so isn't really a straightforward negative aspect, or even a problem.
Erin
So you don't get that same clinical experience [at university], that confidence of being with patients, that you do when you start placement...I mean it was really hard, when I first started I didn't know - I think I'm quite a confident person anyway, so maybe I found it easier than other people, but to just have to suddenly talk to patients, like real patients, and you think, "Oh my goodness, you've actually got a hearing loss, I don't know what to do," and it's very different.
Suggestions
- With everything you have a checklist and you want to do things in this order but then the patient comes in and throws you. Actually when you get more experienced, you can follow the patient and go with the direction they take it, rather than rely on this checklist. It might be that you get more out of them by just having a chat and empathising with them. At the end of the day, they are just people. They are not someone you can't talk to and stick to a list. If they say, they can't hear the TV, you can make them feel comfortable and have a chat with them about what they can't hear
- Observe how other professionals treat patients, talk to and act with them. You can then notice the approaches that work and don't work.
- Erin needs to judge the person she is seeing and find out how they want her to talk to them. Some people prefer facts while others like to talk about how they feel. As it's not immediately obvious what this person prefers, it might be best to give them options by saying, "Would you like me to give you an overview or a detailed explanation of this procedure?"
- While you are still training and learning, it is likely that not all of your appointments will go to plan. Even if you make a minor mistake, that's a good time for you to reflect and learn from it.
Sarah
I tend not to introduce myself as a student, and I think most of us take that approach. No doubt they'll see the badge at some point during the appointment...When we send them clinic reports, it's got that we're a student on the bottom of it anyway, so they will know eventually.
Suggestions
- Sarah should tell them they are seen by a student from the start because they might think they are seeing by a qualified audiologist. And if, during the appointment, you go and get someone for help, then it becomes a bigger issue. Also they should know you are a student from the start, because they have the right to be seen by someone else. And if they say they want to see someone else, you should not question their decision. The whole thing is that you should treat them as how you want yourself or your family to be treated.
- This appears to be a very common among audiology students. It may need a frank and honest discussion with the clinical supervisors - you should find out from them what they want you to do.
Erin
I talked to the head of department and said (...) "Right, this is it, I can't do this anymore," (...). I kind of feel like I have to fight my own battle a little bit of getting my learning done. There's not necessarily someone responsible, making sure that - I mean I have a supervisor, but she's now ill, and then going away for three weeks, so I'm alone for a month, so I have to make sure myself that I get the learning done that I need to.
Suggestions
- If your supervisor is away, there should be someone else taking up that role.
- Students are responsible for their learning portfolio and for their own learning. In terms of your portfolio, and your own learning, and your PDP, you have to just get on with it. You can seek out your supervisor for advice and to show them examples, but staying on top of the work is your responsibility.
- It is really horrendous to be left to one's own devices - but it does happen. It is good that Erin went to talk to her head of department. If she cannot resolve this issue, it should be brought to the attention of the university, either during the pastoral day or during the scheduled phone calls.
- If this happens the advice would be to check out the log book and to make sure that this is up to date. Oftentimes this is left aside, but it can help to orient the student in terms of the kinds of things they should be seeing and doing.
Amanda
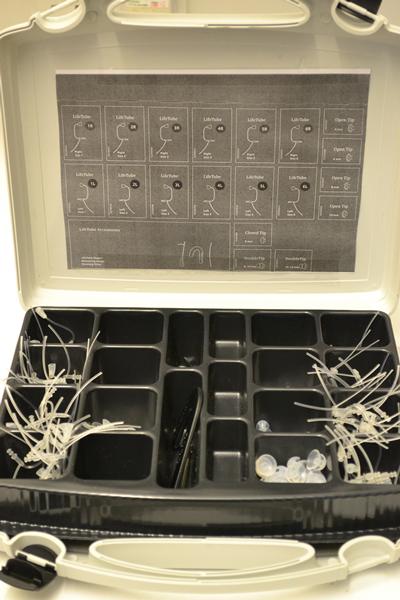
I've said no to a couple of procedures. You have to take, to make the ear mould, you have to put like a little foam stopper into a patient's ear and inject some like soft putty stuff. And there have been a couple of times I've said, "Actually can you do this one? This patient has had surgery," or, "They've got a perforation, I'm not really comfortable doing that." And someone else has done it; they haven't questioned me saying that I don't want to do it.
Suggestions
- Amanda did the right thing by saying ‘no' to something she was not feeling comfortable and competent. She should not be afraid to ask for help. And if someone is in the next room, she should not be afraid to tell the patients, ‘I am going to ask someone from the department to check that for you.' It's fine to do that.
- If someone got to the stage where they are left in a clinic by themselves, it's very easy to think, ‘oh they are expecting me to do the clinics; I can't ask for any help' but that's really not the case. They will usually be someone in the next room and it's okay for you to go and ask them for help.
- When learning these procedures, Amanda might want to start by watching and then ask to be walked through it step by step - with the supervisor present. If the audiologist is simply asked to take over, she will never learn it.
- It will be good for Amanda to put the foam stopper in and look if it's in the right place and then ask her supervisor to check if what she has done is right. In that way it shows she is willing to take a bit of an initiative rather than asking them to do the whole thing. There has to come point where you feel ready to take some small risks and learn from them, otherwise you will not progress as much.
Erin
..in [City] I got to the point within a few months were I had all my own patients and I had my own lists. So I think that's a real downfall of the audiology placement, is that you spend six months really being trained up...and then you just get like plucked out of there, thrown somewhere else. And I understand that when I came here, for kind of safety reasons, they can't just let you loose on a patient, and take [Clinic's] word, "Oh Erin is fine," or whatever. But I feel like I've been here seven weeks now and I've still not seen any patients on my own...you start to feel like you're being deskilled.
Suggestions
- When you switch from one placement to another, you have to take it right back and remember there has to be a settling time again. In that time people will have to judge the level you are in your training before they say ‘Ok, you can do that now.' You can also use your experience of your previous placement to ask intelligent questions such as, "In my last placement we did it this way, what do you do?" In that way, you put across to the team that you do know what you are doing and maybe she can ask to do some more.
- It is easy to think, "They don't trust me and feel you are being deskilled". If you have got the experience, your skills will come through whether you are running a clinic on your own or with someone else.
- It might take time for you to get to know the team and to gain their trust. Perhaps rather than taking a whole clinic on your own, you can ask to do a bit more to show that you can be trusted.
- Erin should discuss this with her new supervisor, explain where she was when she left her last placement, and tell them what she did at her last placement. For example, she can ask to do a hearing test rather than expect to run through whole clinic list.
- I agree that the transition is hard. You've just settled in to your first placement and started to get used to the system and then it's all changed and it almost feels like your back to square one. You probably need to discuss this with your supervisor.