Getting under the skin of allergies
Our researchers are leading the largest study of its kind to improve our understanding of allergies
One in five people in developed countries suffer from an allergy at some point in their lives – and allergies are on the rise. Southampton researchers are leading the largest study of its kind to improve our understanding of allergies.
Leading the way
The University of Southampton has been a strong centre for allergy research for many years, and our Southampton Allergy Centre is recognised as the World Allergy Organization Centre of Excellence for allergy research, clinical service and education.
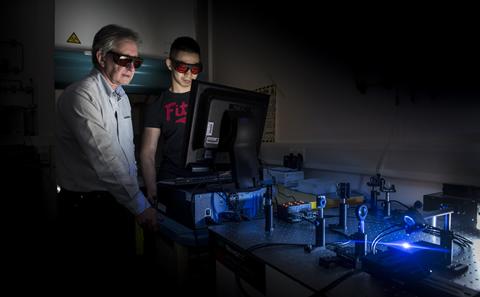
John Holloway, Professor of Allergy and Respiratory Genetics, and Associate Dean, Research for Medicine at Southampton, is leading a team focused on epigenetics – extra messages in the DNA that control the level of gene expression.
“The fascinating thing about them is that they can be added to your DNA in response to an environmental exposure,” explains John. “It could be your mother’s diet while she was pregnant with you, it could be cigarette smoke in the air, which could lead to a chemical change in your DNA that changes the way genes are expressed, and that might increase your risk of disease.”

Southampton is a great place for research and education on allergies and respiratory disease.
Isle of Wight allergy study
One Southampton research team has been studying a particular epigenetic mark, DNA methylation, in the world’s longest running study following people with allergies from birth.
All 1,536 participants of the study were born in 1989 on the Isle of Wight, UK. Every child who was born during a 14-month period on the island was recruited to this study and followed up at ages one, two, four, 10, 18 and 27.
“Our aim is to understand how allergies develop, and this study is the ideal way to do this because allergies develop early in life and they can change over time,” explains study leader Hasan Arshad, Professor of Allergy and Clinical Immunology at Southampton, and Director of the David Hide Asthma and Allergy Research Centre, Isle of Wight.
By looking at the epigenetic markers, the team can predict who is most likely to develop asthma and the environmental factors that are most likely to influence the gene.
Research impacts
The Isle of Wight study has generated more than 100 research papers contributing to our understanding of allergies. Some of this research has translated into policy; Southampton researchers were part of a team that found that introducing peanut into an infant's diet within the first 11 months of life can prevent peanut allergy in those at high risk.
Our Respiratory Biomedical Research Unit has also used links with University Hospital Southampton NHS Foundation Trust to conduct research and develop new treatments, including a monoclonal antibody therapy that is now available to patients with severe asthma. This led to the spin out of drug development and discovery company, Synairgen.
Developing the leaders of tomorrow
At the University of Southampton we are also developing tomorrow’s allergy experts through our MSc Allergy programme, which is designed to give health professionals the skills to treat patients more effectively. As well as a part-time MSc, we also run the only full-time MSc Allergy course in the world.
“Southampton is a great place for research and education on allergies and respiratory disease, both because we are a World Allergy Organization Center of Excellence with a long track record, and our ethos of collegiality, bringing expertise from different disciplines to solve problems,” says John.
Links to external websites
The University cannot accept responsibility for external websites.
Other University of Southampton sites
You may also be interested in:
Copper's role in tackling superbugs
Our researchers have discovered the role that copper can play in eliminating healthcare associated infections (HAIs) and their findings are proving influential across the world.
Personalised sensors for medical tests
Paper-based sensor could test for multiple conditions without the need to visit the doctor.
Beating breast cancer
Examining inherited high-risk genes in order to tackle genetic breast cancer.