Scientists make cancer breakthrough that could improve immunotherapy success rate
University of Southampton scientists have made a breakthrough in understanding why some cancers don’t respond to immunotherapy treatment, bringing fresh hope that many more people could survive the disease.
Researchers, supported by Cancer Research UK, have identified a key cell protein that prevents the treatment from working and crucially, have found a drug that can overcome it.
The findings are published in the journal Cancer Research.
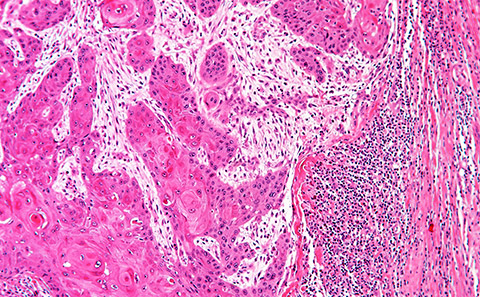
Immunotherapy works by triggering the body’s own immune system or ‘T-cells’ to recognise and attack cancer cells and has been successful in treating many types of cancer. However, for a large number of patients, the treatment is ineffective due to a protective barrier of cells called cancer assisted fibroblasts (CAFs) sitting around the tumour that our T-cells cannot penetrate.
The six-year study, led by Southampton's Professor Gareth Thomas, revealed that the CAFs are regulated by a protein called ATM which normally controls DNA repair in cells. Blocking the ATM protein, prevents the protective CAF barrier forming and therefore gives the patient’s immune system a better chance of attacking the cancer cells while undergoing immunotherapy.

Gareth, a professor of experimental pathology at the University's Centre for Cancer Immunology, said: “Immunotherapy for cancer has been a very exciting development but still doesn’t work in most patients. Our results suggest that in many cases, treatment resistance is caused by CAFs and this can be overcome by targeting ATM.
“Many patients have tumours that contain high levels of CAFS, which are preventing the T-cells from reaching the tumours. This includes around 50 percent of head and neck cancers, 95 percent of pancreatic cancers and 60-70 percent of oesophageal and colorectal cancers.
“If we can prevent this CAF formation by blocking the ATM protein then we can overcome immunotherapy resistance and we are very excited that this could be effective in a large group of patients across different cancer types.”
What makes this latest study even more significant is the fact researchers have already designed a drug that can block the ATM protein. ATM inhibitors have been developed for another purpose – to sensitise cancer cells to radiotherapy and are currently being evaluated in clinical trials for their potential to improve radiotherapy response in people with brain cancer.
Professor Thomas said: “What’s really exciting about this is that we’ve been using a drug that already exists, so we don’t need to spend time developing a drug and could take this straight to testing.
“It is very effective at getting T-cells into the tumour by targeting CAF, which is a completely novel use for the drug. We've shown in our mouse models that we can inhibit CAF formation, overcome immunotherapy resistance and significantly improve the response to this type of treatment. It is really very striking.”
The team’s next step will be to develop a clinical trial that will see the research translate from bench to bedside.
Reflecting on the six-year study, Professor Thomas said: “Research is a real roller coaster. There are lots of highs and there are also lots of lows. But when something does come together, you're excited because you think perhaps it could make a difference that makes it all worthwhile and we're very excited about this.”
Michelle Mitchell, Chief Executive of Cancer Research UK said: “Immunotherapy is an incredibly exciting area for the treatment of many cancers, but resistance to immunotherapy remains common. It can be hard for patients to undergo treatments, which may come with challenging side effects, knowing that there is a chance that they may not work.
“Research like this, that offers insights into how resistance to immunotherapy works, and how we might overcome it could lead to better chances for patients undergoing these types of treatments.”
This latest research was led by scientists from the Faculty of Medicine at the University of Southampton, working with colleagues at the universities of Leicester, Liverpool and Centre Médical Universitaire, Switzerland, together with AstraZeneca in Cambridge.
