Tell us about your current research focus and why did you decide to focus your career on that particular area of research?
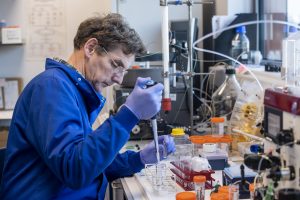
Our team are highly focused on antibody therapeutics. These molecules are generated naturally in the body to fight infection and we take advantage of their fantastic design features to fight cancer.
I have always been fascinated by Biology and how the immune system works, with a similar interest in how cancer develops and how we might make better treatments. Antibodies sit right at the heart of these questions. In the last 20 years and especially within the last decade, antibodies have become increasingly important for treating cancer but there is still so much to do and understand to make them even more effective.
Professor Cragg,Antibodies have become increasingly important for treating cancer but there is still so much to do and understand to make them even more effective.
How does your team generate antibodies?
We generate antibodies in a variety of ways. The first antibodies used to treat patients were generated using a technology called Hybridoma Fusion. Here, mice are immunised with the molecule that we wish to generate antibodies to. The mice mount an immune response and generate lots of antibodies. We then take the cells that make the antibodies (B cells) from the mice and fuse them with an immortal cancer cell called a myeloma. We select those cells that have fused and are secreting the antibodies that we want. This creates an immortal cell called a hybridoma that secretes a single antibody (called a monoclonal antibody). We can then take the genetic material from these cells and manipulate it in the lab to make it more human. Initially we did this by a process called chimerisation (making them about 75% human rather than murine) or more typically now, humanise them, replacing almost all of the mouse sequence. Both of these types of antibody are approved for use to treat cancer.
More recently, we have developed laboratory methods to generate antibodies, without needing the mouse immunisation step. This technique uses human genetic material from human B cells and displays the various antibody components on a virus called a bacteriophage. Each Phage encodes the genetic material to express a different antibody molecule and when we want a new antibody to bind a new target we ŌĆ£fishŌĆØ for the phage that bind. We than take that genetic material and manipulate it as above to make complete, fully human, antibodies. This is exactly how the antibody BI-1206 was made by our collaborator BioInvent International , which is currently in clinical trials.
How could your research change the way cancer is treated?
We have a number of different antibody approaches at the Centre. If we can find the right one for the right cancer, coupled to our ability to develop clinical trials, we have the potential to really make a difference.
YouŌĆÖve recently started a new collaboration with South Dakota State University, examining how macrophages, recognize and destroy target cells and why they sometimes do not ŌĆō how important and exciting is this new project?
Alongside Professor Stephen Beers, and a team of other colleagues in Cancer Sciences, we are already studying macrophages and trying to find ways of making them better at attacking cancer cells, but the new collaboration forges an alliance with experts in the US that use cutting-edge CRISPR gene-editing tools to identify which genes promote or inhibit the macrophages. We donŌĆÖt have this expertise in Southampton, so it gives us some fantastic new opportunities to grow our understanding and do the very best science. This is a really exciting and important step forward in the cancer research taking place in Southampton.
Professor Cragg,If we can find the right one for the right cancer, coupled to our ability to develop clinical trials, we have the potential to really make a difference.
You are the director of the UniversityŌĆÖs i4PhD Cancer Immunology Pathway ŌĆō tell us a bit more about this opportunity for PhD students?┬Ā
By bringing together access to cutting-edge immunology research and excellent transferrable skills training, it provides everything the next generation of cancer immunology leaders could want. For example, it has lots of fantastic training in the first year, exposing the students to the newest types of experimental techniques such as bioinformatics and systems biology, coupled to expert immunology teaching. The students then do three separate projects in different labs to expand their experience and expertise and after that develop the project they will pursue for their main PhD in years 2 to 4. The focus of the studentsŌĆÖ project is up to them ŌĆō to follow whatever inspires and drives them.

As you know the Centre was funded entirely through philanthropic donations and the Cancer Immunology Talent Fund (CITF) continues to fund our research and train the next generation of researchers. As a scientist, how important is to have such support for medical research?
It is becoming essential. The charity sector has been massively hit by the COVID-19 pandemic with CRUK alone reporting a loss of more than ┬Ż150m in funding for this year (2020). The University sector has been similarly impacted, reducing their ability to support our work with infrastructure and so funds like the CITF are becoming increasingly important to allow us to continue to operate at the highest level.

What do you think the future holds for cancer immunotherapy?
Despite the current issues in the world, the cancer immunotherapy community continue to learn more about how cancer and the immune system co-evolve, and this knowledge provides us ever-greater possibilities to intervene with new treatments. Two decades ago we didnŌĆÖt have antibody drugs for treating lymphoma and leukaemia patients ŌĆō they are now used in first-line treatment. One decade ago we didnŌĆÖt have checkpoint blocking antibody drugs ŌĆō these are now able to cure a proportion of very difficult to treat solid cancer patients for which we didnŌĆÖt have any other options. I am very optimistic we will continue to make progress and improve understanding of cancer and thereby develop better and more effective treatments.
What would you say is your proudest career achievement?
I was awarded the Vice ChancellorŌĆÖs Award for Research Impact in 2017.
Professor Cragg,I am very optimistic we will continue to make progress and improve understanding of cancer and thereby develop better and more effective treatments