Tim Fenton, Associate Professor in Cancer Biology, joined the Centre for Cancer Immunology at the beginning of 2022. He is currently studying a group of seven genes called APOBECs and their role in how successful cancer treatments are in patients.
Can you explain what your research focuses on?
APOBECs protect us from viral infection by attacking viral DNA, but they are also responsible for causing the mutations in cells that can drive cancer development and that can cause cancers to become resistant to treatment.
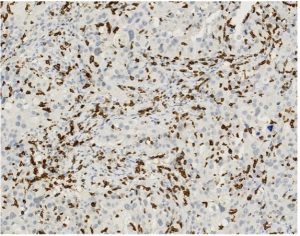
We are interested in learning how APOBECs go rogue in cancer cells, including how its activity is influenced by the tumour microenvironment and conversely, how the mutations it generates affect how our immune system can recognize and respond to cancer cells.
Our work is primarily funded by the Biotechnology and Biosciences Research Council (BBSRC), Cancer Research UK and the Rosetrees Trust
What impact could your research have on cancer patients?
My hope is that by understanding how APOBECs enable cancer cells to become resistant to treatment, we may be able stop this process in patients undergoing treatment and therefore to prevent their tumours from recurring. We are also trying to determine whether knowing a particular APOBEC gene is active in a patient might enable the design and deployment of improved cancer vaccines.
What impact could your research have on the field of cancer immunology?
One major limitation of current mouse models of cancer is that they typically lack the genetic complexity of human cancers. A key aspect of our work is the development of a new mouse model, which contains the seven human APOBEC genes, which we predict will allow us to model more ŌĆśhuman-likeŌĆÖ tumours.
We think this will have significant benefits for studying anti-tumour immune responses in mice and for testing the likely effectiveness of new cancer immunotherapies before moving into clinical trials. In collaboration with Dr Chris Hanley and with generous funding from the CCI Talent Fund, we have begun by generating a new and unique lung cancer model in our humanised APOBEC mice.
┬Ā
Understanding how cancers become resistant to systemic treatments and learning how to prevent this from occurring is, in my opinion, crucial if we are to improve the prospects for those patients unfortunate enough to be diagnosed with advanced stage cancer.
Why did you decide to focus on that particular area of research?
Systemic cancer treatments (including chemotherapy, ŌĆśtargetedŌĆÖ therapies in which specific mutated proteins in cancer cells are inhibited and now immunotherapies) are used when a patientŌĆÖs cancer has grown too large or spread too far beyond the site from which it arose to be treatable by surgery or radiotherapy alone. These therapies can be remarkably effective at first but sadly all too often, after a period of months or years, the cancer returns and at this point, it is resistant to treatment. Understanding how cancers become resistant to systemic treatments and learning how to prevent this from occurring is, in my opinion, crucial if we are to improve the prospects for those patients unfortunate enough to be diagnosed with advanced stage cancer.
Having worked on a molecular mechanism that drives treatment resistance in brain tumours during my postdoctoral research in California, I was keen to continue working in this field upon returning to the UK in 2011. At that time, when I began working in Chris BoshoffŌĆÖs CRUK Viral Oncology group at UCL Cancer Institute, it was becoming increasingly apparent that a form of throat cancer that is caused by the human papillomavirus (HPV) was affecting a rapidly growing number of people in the UK. This cancer mainly occurs in the tonsils and unusually for throat cancer, it affects non-smokers. When we discovered that the APOBEC genes, which should help protect us from HPV infection can actually help fuel the development of these HPV-driven cancers, it really caught my scientific curiosity, and I became fascinated with how our innate immune response to viral infection might turn against us in this way.
It has since become clear that APOBEC genes play a role in many other cancer types, including those (e.g. lung and breast) with no apparent viral link, and crucially, that they drive the development of resistance to cancer drugs. This is a relatively new field; there is much still to learn and, I feel, a good opportunity to make meaningful contributions in the coming years.
Why did you decide to work at Southampton and in particular the Centre for Cancer Immunology?
The University of Southampton is internationally renowned for its work in the field of cancer immunology, and I was well aware of its reputation for many years before coming here. As my work in cancer research drew closer to the interface with immunology during my time at UCL, I began collaborating with Professor Gareth Thomas in the School of Cancer Sciences and the CCI. We published several papers together over the years and during my visits, I was particularly impressed by the proximity of the researchers to the hospital and by the way in which translational cancer research is conducted here. We are living through a time of remarkable progress in the development of cancer immunotherapy and the CCI is a clear demonstration of SouthamptonŌĆÖs prominence in this field. When I saw that the department was recruiting a molecular cancer biologist to run a research group here, I was excited by the prospect and was fortunate to be successful in securing the role. Although it was quite an upheaval for us to move as a family from Kent, weŌĆÖve settled very well on the south coast and I am delighted that I moved my research here.
What is your long-term goal?
IŌĆÖd like to see a discovery we have made in my lab be incorporated into a new and more effective strategy for treating cancer patients. This might involve being closely involved in developing a drug against a new target we have identified or seeing knowledge we have generated being used to devise more effective combinations of existing treatments for patients. These aims are very well supported at Southampton, with the colocation of the CCI, the Experimental Cancer Medicine Centre and the Clinical Trials Unit providing a clear path to translation of our research. As a member of the executive committee for the British Association for Cancer Research, I am also keen to ensure that we foster a sense of community among cancer researchers in the UK, including support and opportunities for students and early career researchers.
What excites you most about the future of your research field?
This is an incredibly exciting time to be a biological/medical scientist. Our ability to sequence DNA and RNA at massive scale and relatively low cost is affording unprecedented insight into the changes that happen in cancer cells, and in the cells around them ŌĆō the tumour microenvironment. With the ability to extract more and more information from tumour samples and to use gene editing techniques to build more refined models of cancer in cells and mice, we are able to ask bigger questions and to get answers more quickly than ever. I am hopeful for significant and much-needed progress on screening and early diagnosis of cancer over the coming years and for those who do develop advanced cancers, our ever deeper understanding of how the immune system can be re-awakened with antibodies and vaccines promises to deliver much better outcomes.
I am hopeful for significant and much-needed progress on screening and early diagnosis of cancer over the coming years.