‘Crown-like structures’ surrounding breast tumours in overweight and obese patients could hinder their response to therapy, a new Southampton study has found.
The findings of could potentially be used to improve personalised treatment for patients with HER2 positive overexpressed breast cancer.
The study, was led by Professors Stephen Beers, Ramsey Cutress and Dr Charles Birts at the Centre for Cancer Immunology, and published in Scientific Reports . It was funded by grants from Against Breast Cancer, Cancer Research UK, Breast Cancer Now and World Cancer Research Fund UK.
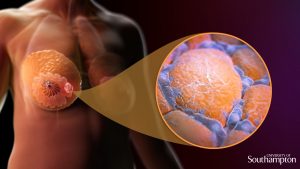
Adipose tissue, or body fat, is an important component of the healthy human breast and yet high body mass index (BMI) is associated with increased risk of developing breast cancer. Overweight patients also have worse survival rates than patients with healthy body weight.
In patients with a high BMI, increased body fat surrounding the breast can cause inflammatory immune cells, called macrophages, to gather in the breast’s fat tissue. These macrophages can then form what are called ‘crown-like structures’ by surrounding these fat cells (see picture below). This creates an inflammatory environment in the breast which can lead to the onset and growth of tumours.
How these crown-like structures go on to affect breast cancer progression and respond to therapy is largely unknown.
Scientists at the Centre for Cancer Immunology assessed samples from a group of HER2 positive breast cancer patients to investigate the link between high BMI and the formation of crown-like structures, and the subsequent effect of these on how patients responded to therapy with a drug called trastuzumab (Herceptin®).
They showed that patients who were overweight or obese had significantly more crown-like structures in their fat tissue surrounding the tumour and that this was associated with a faster time to metastatic disease – an indication of how well the patients have responded to therapy.

They then went on to identify a potential molecular biomarker, called CD32B, on the surface of the macrophages in these crown-like structures. When this marker was present in overweight and obese patients, their response to trastuzumab therapy was poorer.
Stephen Beers, Professor of Immunology and Immunotherapy at the University of Southampton said “These findings will be of interest to clinicians and researchers involved in breast cancer treatment as they could potentially be used to develop personalised treatment for patients with HER2 positive overexpressed breast cancer.
“For example, doctors would know that patients with a high BMI and the marker on their crown-like structures are likely to have a poor response to trastuzumab therapy. They may therefore benefit from more intensive anti-HER2 therapy earlier in their treatment.
“On the other hand, this study highlights how effective trastuzumab treatment is in patients that do not have the marker. So these patients could benefit from a lower dose of anti-HER2 therapy which may minimise the side-effects they experience. Further studies with more patients will be needed to help confirm these initial findings.”
The team is now looking at ways to change the behaviour of these crown-like structures to improve responses to breast cancer therapy.