Paper-based medical diagnostic sensors will allow rapid and affordable point-of-care medical diagnostics.
Overuse of broad spectrum antimicrobial agents means that resistance to them can evolve rapidly in microbe populations, so that when the broad spectrum treatment is really crucial, it is less effective at saving the patient. Multi-drug resistant Gram-Negative Bacteria (GNB) such as such as E-Coli, Klebisiella, Pseudomonas species, are a major health problem and their growing resistance to multiple antibiotics poses a clinically significant challenge in hospital medicine.
Early diagnosis and prompt correct antibiotic treatment is important for clinical recovery and prevention of this serious antibiotic resistance. Current routine empirical antibiotic therapy protocol for diagnosis of such pathogens involves laboratory based urine bacterial culture testing which can take up to 2-3 days, and when a culture is deemed positive, further susceptibility testing is done to guide antimicrobial treatment. Since the results for the antibiotic resistance pattern are almost inevitably unavailable for this substantial period of 2-3 days, the only option available to the clinician is the treatment of the patient using an empirical antibiotic prescription. Such treatments can either prove to be ineffective, or potentially worsen the patient’s condition. If the bacteria are resistant, it can exacerbate the prevalence of antibiotic resistance.
However, if the specific microbe species causing an infection can be quickly identified it will allow doctors to prescribe a specific targeted antimicrobial instead of using a broad spectrum antimicrobial. So we need rapid diagnostics. We also need affordable and easy-to-use diagnostics, because cash and training can be in short supply in many health crises around the world.
Therefore this project is using laser technology to research into the development of a paper-based diagnostic, resembling the paper-based 'dipstick' technology of pregnancy testing kits, that will allow the detection of multiple pathogens in urine, whether in the clinic or in the community.
How do we make the sensors?
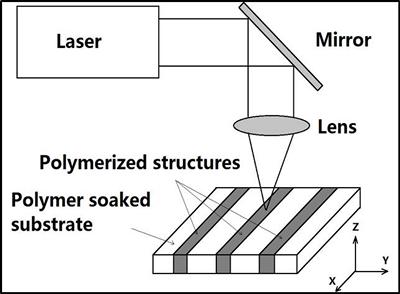
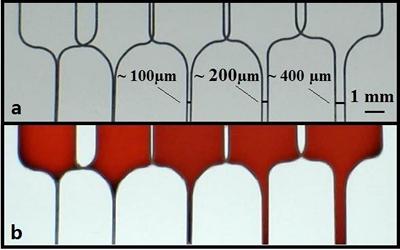
The sensor relies on the implantation specific polymer chemicals into small channels in the paper. The chemical building blocks of these polymers are implanted in the channels, and then a laser is fired onto these channels, causing the chemical building blocks there to join up and bond to form the required specific polymer. The smallest channel widths that can guide fluids are about 100 microns. Each channel can then help tell us what microbe species are present.
NAMRIP Members: Professor Robert Eason and Dr Collin Sones, Optoelectronics Research Centre, Faculty of Physical Sciences and Engineering
Rob Eason and Collin Sones are working with clinician Bhaskar Somani, from the Faculty of Medicine. Dr Somani is a prominent endo-urologist and is a core member of the Catheter research group which regularly battles infections caused by kidney stones, ureteric stents and catheters. A simple and reliable Point Of Care (POC) test would greatly aid him in screening patients who have undergone surgery for resistant bacterial infections. Another researcher on the project is Professor Bill Keevil from the Centre for Biological Sciences in the Faculty of Natural and Environmental Science, who will provide the expertise in the development and implementation of biochemical assays on the proposed laser-patterned laser fluidic devices (LFDs).