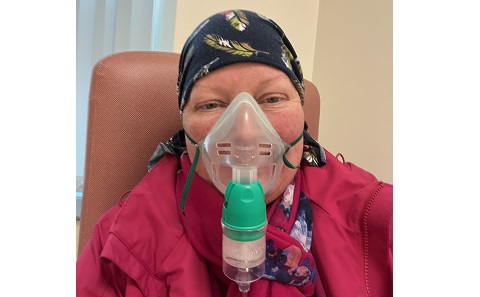
Patient with rare lymphoma of the brain says she’s proud to be part of research that is Standing Up To Cancer

A lymphoma patient who is taking part in a clinical trial funded by Stand Up To Cancer says she’s grateful to have the opportunity to help further research and find better cures for a rare form of the disease.
Caroline Palmer is taking part in the OptiMATe trial, which is being run by the Southampton Clinical Trials Unit.
Caroline, 48, was diagnosed with primary central nervous system lymphoma (PCNSL) in April this year.
“It was by shear accident that it was found. I had a bit of a migraine which I thought was due to perimenopause and the fact that I’m a teacher of four and five-year-olds, so I expect to get a few headaches. I went to the optician, and they found I had a slight bleed behind my eye and a swollen optic nerve.”
Caroline was sent to for an MRI and staff at the hospital then told her she needed to go to A&E.
“I still felt fine because I didn’t think there was anything the matter with me, it was just a bit of a headache. But at midnight that night they came and told me I had a brain lesion.”
“I was in hospital for 10 days, being tested from top to toe. I was then told I needed a brain biopsy and was transferred to a larger hospital.”

Eventually, Caroline was transferred again to an isolation room to keep her from catching anything, and it was then that she was told she had primary central nervous system lymphoma.
“I’d never heard of it. I’d heard of cancer and leukaemia, but I didn’t realise that this was blood cancer. And I felt like maybe I only had a bit of it because I still felt ok, but I then found out I was actually very poorly, and I realised that this is a very deceitful disease.”
Treating PCNSL
Primary central nervous system lymphoma (PCNSL) is a type of blood cancer that affects the brain and can be a difficult cancer to treat.
The standard treatment for PCNSL is called MATRix, a combination of chemotherapy drugs and an immunotherapy treatment called rituximab, followed by a stem cell transplant.
A previous trial found that MATRix followed by consolidation with high-dose chemotherapy and stem cell transplant could lead to long-term survival for around 70% of PCNSL patients under 70 years old, and led to a change in the guidelines for treating the disease in the UK and much of Europe.
However, in around a third of patients MATRix treatment is not successful. The OptiMATe trial is an international collaboration which is investigating whether MATRix can be optimised by changes to the timings and intensity of how the different drugs are given.
Following her diagnosis, Caroline was straight away offered the chance to take part in OptiMATe.
“My best friend is a nurse and she had already said to me that if I was offered any sort of clinical trial I should consider it. So, I took all the information and read it and it scared me a bit, but the information about the standard treatment scared me too. So, I decided pretty quickly that I would do the trial.”
“When I had my first chemo, I cried. Because you think immediately that all your hair is going to fall out and you’re going to be really poorly. But it didn’t happen for weeks, and I think I went through a denial because a lot of other people in the hospital looked really sick and I felt fine and was walking around. But then I realised that I was getting weaker and weaker and more fatigued.”
“The doctors are very open with you about how it will be, and that you will be poorly. And the research nurses are amazing. You can phone any time and just get things explained. I was in a better place because I knew what was happening.”
Helping find the treatments of the future.
Caroline is one of six PCNSL patients who have so far been recruited to the OptiMATe trial here in the UK.
And she says having the opportunity to be part of a clinical trial and help with research into the disease means there is something positive to come out of her situation.
“I just feel extremely grateful and lucky that I’ve got the opportunity to be on the trial. This disease is horrible, and I want to do anything I can to make this easier for somebody else. Trials like this will hopefully mean people in the future have an easier recovery than I’ve had.”

And Caroline says having her husband Wayne and 10-year-old son Isaac with her every step of the way has been a huge support, but that it has been hard on all of them.
“Isaac’s finding it tougher now I’m home. He missed me when I was in hospital. He wasn’t meant to get a phone until he was eleven, but he needed to be able to call me when he wanted. And now I’m home he can see what’s happening. I look fine and well, but I’m still struggling, I’m still being sick, it takes me a while to get up the stairs and he sees that.”
“It’s been hard, but I’ve got to get through it. I have no choice but to be positive and get on with it.”
And Caroline is always taking the positives from her treatment and from being part of the trial.
“I’m getting my eyelashes back now, just baby ones, but it’s so nice to see them coming back. And the fact that the trial is funded by charity is amazing. I saw SU2C programmes on TV this week with the celebrities sleeping on the side of a mountain and I thought, “Wow, I’m part of this!”
“The more people that I can help, the better. What I’ve been through is tough, and hopefully by me doing the trial and other people being involved in trials the researchers will get enough data to figure out faster, better ways to treat this disease. A couple of years ago, none of this was here, so I’m lucky thanks to previous research and I want to help others in the future.”
The OptiMATe trial
The OptiMATe trial is an international research project, led by a research team in Germany. The trial being led in the UK by Professor Chris Fox, Consultant Haematologist at Nottingham University Hospitals NHS Trust, and run by the Southampton Clinical Trials Unit (SCTU).
“Despite huge advances in treatments for patients with PCNSL in the last few years, there are still many patients whose lymphoma does not respond to, or returns following, current treatment approaches,” says Professor Fox. “We hope that the OptiMATe trial will be able to provide evidence that this new and optimised treatment strategy can provide an alternative treatment pathway leading to improved survival for patients.”
There are currently eight hospitals in the UK running the OptiMATe trial, with a further eight due to open in the coming months. The trial is also recruiting patients at hospitals in Germany, Italy and Austria.
The trial is also looking to analyse biological samples and MRI imaging to try and identify patients who may be at higher risk of their Lymphoma not responding to treatment or returning after their treatment has finished.
The UK arm of the trial is funded by just over £1m from Cancer Research UK’s Stand Up To Cancer campaign and is sponsored by Klinikum Stuttgart.
.jpg)