Intelligent prosthetic liners could ease pain for lower limb amputees

A new device could help to relieve the pain and discomfort experienced by thousands of amputees as a result of poorly fitting replacement lower limbs. Researchers are developing a prototype of the world’s first prosthetic ‘intelligent’ liner with integrated pressure sensors, which could be available to NHS patients in as little as three years.
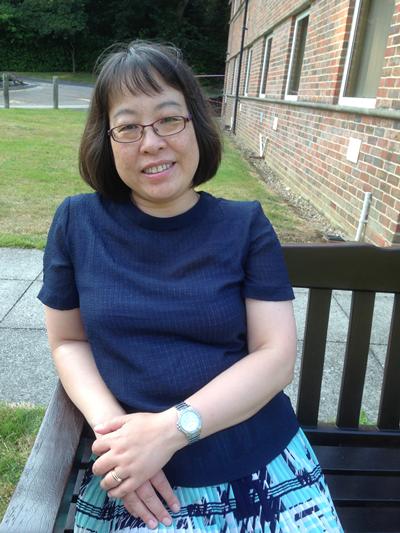
The sensors for the device, invented by Dr Liudi Jiang and an interdisciplinary team at the University of Southampton, measure the pressure and pulling forces at the interface between a patient’s stump and socket of their prosthesis. In excess these pressures in excess can cause tissue damage, leading to painful sores.
Dr Liudi Jiang said: “Socket fit is the single biggest factor determining whether prosthesis will be successful for a patient. If we had a simple way to accurately measure the load at the socket-stump interface and determine the best possible fit for that limb, it would completely transform the socket fit experience for amputees.
“We’re hoping that the development of the intelligent liner will be the first step leading to the ‘holy grail’ in prosthetics – a fully automatic, self-adjusting smart socket interface for amputees.”
Dr Jiang is part of a multidisciplinary team at the University of Southampton, which also includes Professor Dan Bader, an expert in tissue biomechanics and developing sensors designed to assess skin health.
Professor Bader said: “Mechanical forces during physical activities of the amputee can lead to breakdown of soft tissues at the stump, which can prove very difficult to heal and will inevitably result in distress for the patient.”
There are 50,000 lower-limb amputees in the UK, most of whom use artificial limbs that are attached to the residual limb through a socket. No two stumps are exactly the same shape and size and even an individual’s stump can change shape over the course of a single day.
Pain, discomfort and ulceration are frequently experienced at the socket interface due to poor fit. This stems from the excessive build-up of pressure within the limb socket (causing high ‘loads’ on the stump).
Synthetic liners, worn like a sock over the stump, provide some cushioning against the hard socket, but at present there is no convenient way to accurately measure the critical loads at this interface in the clinic. Without this information, prosthetists face difficulty in fitting replacement limbs and the outcomes for patients are variable.
The intelligent liner will allow clinicians to quickly and accurately assess and optimise socket fit at the outset. The wireless interface will also monitor changes to socket fit over time, alerting patients of the need to adjust their socket or activities to prevent ulcers from forming. This relatively practical and potentially low-cost solution could substantially reduce amputees’ follow-up visits to their rehabilitation centres, giving them a better quality of life and at the same time reducing healthcare costs.
In future, the scientists believe the technology could form the basis for other intelligent materials, for example shoe insoles to prevent diabetic foot ulcers, or mattresses and wheelchairs that protect against pressure sores in immobile or elderly patients.
The Southampton team will work with a leading British company, Chas A Blatchford & Sons Ltd, to fine-tune the design and develop the sensor into a range of thin prosthetic liners to fit sockets of any shape and size.
Dr David Moser, Head of Research at Chas A Blatchford & Son Ltd, who are partners of the research project, said: “This is a tremendously exciting project which has the potential to transform socket technology as a whole in lower limb prosthetics. We anticipate that from the development of this technology we will reach a new level of understanding and uncover the as yet unclear ‘dynamic’ qualities of limb loading and socket fit. This step is crucial for the development of the next generation of socket technology products and future artificial limb controls.”
The work is being funded through the Biomedical Catalyst – a programme jointly managed by the Medical Research Council and Technology Strategy Board that supports innovative ideas from conception through to early commercial development.
Dr Chris Watkins, Director of Translation and Industry at the MRC, said: “The Biomedical Catalyst aims to bridge the gap between promising scientific ideas and commercial development. By helping academic researchers to forge productive relationships with UK business, we are helping to speed up the delivery of new treatments and technologies to those that need them most.”