Study shows beneficial effects of blocking brain inflammation in an experimental model of Alzheimer’s
A University of Southampton-led study has found that blocking a receptor in the brain responsible for regulating immune cells could protect against the memory and behaviour changes seen in the progression of Alzheimer’s disease.
The research, published today in the journal Brain, was jointly funded by the MRC (Medical Research Council) and Alzheimer’s Research UK.
It was originally thought that Alzheimer’s disease disturbs the brain’s immune response, but this latest study adds to evidence that inflammation in the brain can in fact drive the development of the disease. The findings suggest that by reducing this inflammation, progression of the disease could be halted.
The team hope the discovery will lead to an effective new treatment for the disease, for which there is currently no cure.
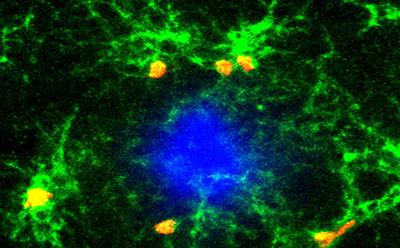
The researchers at the University of Southampton used tissue samples from healthy brains and those with Alzheimer’s, both of the same age. The researchers counted the numbers of a particular type of immune cell, known as microglia, in the samples and found that these were more numerous in the brains with Alzheimer’s disease. In addition, the activity of the molecules regulating the numbers of microglia correlated with the severity of the disease.
The researchers then studied these same immune cells in mice which had been bred to develop features of Alzheimer’s. They wanted to find out whether blocking the receptor responsible for regulating microglia, known as CSF1R, could improve cognitive skills. They gave the mice oral doses of an inhibitor that blocks CSF1R and found that it could prevent the rise in microglia numbers seen in untreated mice as the disease progressed. In addition, the inhibitor prevented the loss of communication points between the nerve cells in the brain associated with Alzheimer’s, and the treated mice demonstrated fewer memory and behavioural problems compared with the untreated mice.
Importantly, the team found the healthy number of microglia needed to maintain normal immune function in the brain was maintained, suggesting the blocking of CSF1R only reduces excess microglia.
What the study did not find is a correlated reduction of the number of amyloid plaques in the brain, a characteristic feature of Alzheimer's disease. This supports previous studies that argue other factors may play more of role in cognitive decline.
Dr Diego Gomez-Nicola, lead author of the study and an MRC New Investigator Research Grant (NIRG) fellow at the University of Southampton, said: “These findings are as close to evidence as we can get to show that this particular pathway is active in the development of Alzheimer’s disease.
“The next step is to work closely with our partners in industry to find a safe and suitable drug that can be tested to see if it works in humans.”
Dr Rob Buckle, director of science programmes at the MRC, added: “It is increasingly clear that inflammation is a key player in a number of neurodegenerative conditions and this study is beginning to unravel the biological processes behind this link.
“The study is an excellent example of how basic research can lead to promising partnerships with industry that could be of real benefit for those with dementia.”
Dr Simon Ridley, Director of Research at Alzheimer’s Research UK, said: “This work, looking at the role of the immune system in Alzheimer’s disease, suggests that blocking the action of the CSF1R protein in mice could help limit the damaging effects of inflammation and protect against symptoms like memory loss. In the last few years, scientists in Southampton have been at the forefront of research into the role of the immune system in Alzheimer’s, so it is encouraging to see this study taking these ideas forward by identifying a specific mechanism that could be a target for future treatments.”
Dr Gomez-Nicola and his colleagues at the University of Southampton will continue their work with funding from the Dementia Consortium – a collaboration between Alzheimer’s Research UK, MRC Technology and pharmaceutical companies, Eisai and Lilly.